- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Click to find the locations nearest youFind locations by region
See all locations -
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Child Life 101
Wednesday, June 12, 2024Join us to learn about the work of a child life specialist, including...
-
Research & Innovation
- Overview
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.


Gynecology
Müllerian Anomalies
We see more, treat more and heal more kids than any other hospital in the region.

What is a Müllerian anomaly?
The Müllerian structures are the structures found in the female fetus that eventually develop into a woman's reproductive organs. These structures were named after German physiologist Johannes Petrus Müller.
During typical fetal development, two tube-like structures called the Müllerian ducts fuse together to create the uterus, fallopian tubes and majority of the vagina. When one of these structures does not fully develop, a malformation of the uterus or vagina occurs, and this is referred to as a Müllerian anomaly. An anomaly that affects the uterus is called a uterine anomaly.
The various malformations are categorized based on the portion of the uterus or vagina that does not form properly, known as:
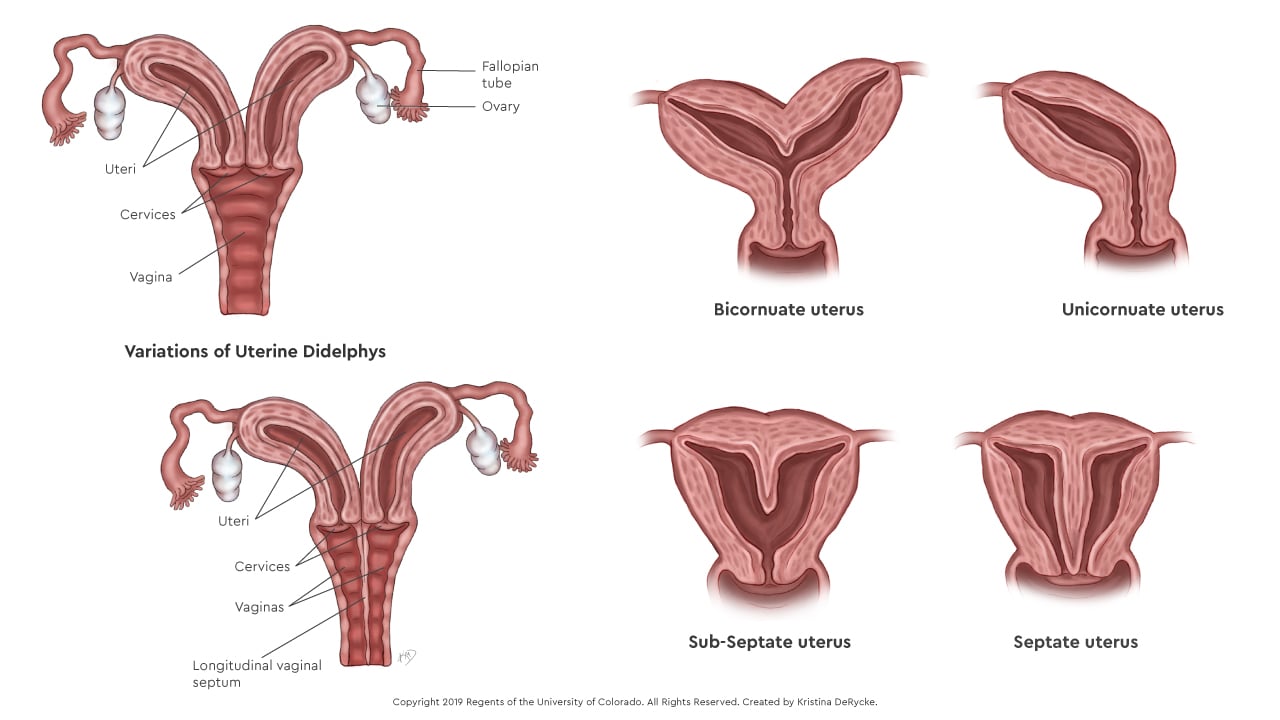
- Septate uterus: The external shape of the uterus is normal, but the cavity is divided by an extra wall of tissue called a septum, which runs down the middle of the cavity. If the septum completely divides the cavity, it is known as a septate uterus; if it partially divides the cavity, it is known as a sub-septate uterus.
- Bicornuate uterus: The external shape of the uterus is abnormal with a large indentation in the fundus (the top of the uterus), which causes the upper cavity to further divide into two cavities. This is a result of the two Müllerian ducts only partially fusing together.
- Unicornuate uterus: Only half of the uterus develops, which is the result of only one Müllerian duct developing.
- Uterine didelphys: The entire uterus and cervix is duplicated (also called a didelphic uterus), which creates two uteri and two cervices. The patient still has the standard two fallopian tubes and two ovaries. This condition is the result of the two Müllerian ducts developing, but not fusing together at all.
What causes a Müllerian anomaly?
Doctors don't completely understand the cause of Müllerian anomalies. They are considered multifactorial, meaning they are likely caused by defects in multiple genes, with some influence from factors in our environment. The reproductive organs begin to develop when the mother is about six weeks pregnant, while an early fetus is developing inside the mother's womb, or uterus.
The reproductive organs begin to develop when the two Müllerian ducts start to migrate toward each other and begin to fuse in the middle of the fetus. Typically, some of the tissue migrates upwards to form the uterus and fallopian tubes, and the remaining tissue migrates downwards to form the vagina. Any disruption in this process may result in a malformation of the uterus, vagina, or both, which leads to a Müllerian anomaly.
Who gets a Müllerian anomaly?
These malformations can happen to any woman, and they occur in about 3 to 5% of the general population. There are no specific known risk factors that cause this condition.
What are the signs and symptoms of a Müllerian anomaly?
Oftentimes, a patient does not have any symptoms, particularly if the uterus and vagina are patent, meaning there is no obstruction to the normal flow of menstrual blood. However, if a septum (extra wall of tissue) is present and blocks menstrual flow, patients can have symptoms of abdominal pain in the absence of menstrual bleeding, at an age when we would expect a girl to be having her monthly period.
Certain uterine anomalies, including a septate uterus, can cause recurrent miscarriages, so a miscarriage may be the first indication that a problem exists with the uterus. Finally, some malformations of the uterus, including bicornuate uterus, unicornuate uterus and uterine didelphys, may not be discovered until pregnancy, when a routine ultrasound shows a malformation. These conditions can also lead to the premature delivery of a baby, in which case the early delivery may be the first sign of the uterine malformation.
What tests are used to diagnose a Müllerian anomaly?
At Children's Hospital Colorado, we use a 3-dimensional ultrasound, magnetic resonant imaging (MRI) or both to take images of the pelvis and evaluate the size and shape of the uterus. An MRI uses magnets to produce detailed images of the body's organs and structures, while a 3-dimensional ultrasound uses sound waves to produce images of internal organs. For the ultrasound, we move a probe along the outside of the abdomen or pelvis to see the internal images. For the MRI, the patient simply needs to lay still as the machine scans the body.
In cases where the Müllerian anomaly is associated with malformations of the skeletal system or the urinary tract, we use X-rays and additional imaging of the kidneys to diagnose the extent of the anomaly. An X-ray uses radiation to show images of solid structures inside the body.
Why choose us for these imaging tests?
Müllerian anomalies are uncommon conditions, and the differences between each type of malformation can be subtle. Receiving the correct diagnosis is critical for patients to choose the right medical and surgical treatment.
Given the rarity of these conditions, it is important that the radiologist is familiar with these malformations. Because Children's Colorado is a regional referral center for Müllerian anomalies, our radiology team sees more of these cases and has the proven expertise and experience required to accurately diagnose them.
How do we make a diagnosis for a uterine anomaly?
At Children's Colorado, we can usually diagnose a Müllerian anomaly by reviewing a patient's imaging tests and medical history. Occasionally, we need to perform a full exam of the pelvic structures to formulate the best treatment plan. To limit any discomfort, we recommend performing this exam while the patient is asleep under anesthesia.
How is a Müllerian anomaly treated?
Treatment for a Müllerian anomaly depends upon the specific condition.
If the Müllerian anomaly is associated with a vaginal septum that is obstructing menstrual flow, we will need to perform a surgical resection (removal) of the vaginal septum.
If the anomaly is a septate or subseptate uterus, we may recommend surgery to prevent miscarriages or premature deliveries. This treatment requires outpatient surgery with a hysteroscope and the resection of the uterine septum. During hysteroscopy, we place a small camera called a hysteroscope through the cervix and into the uterine cavity, which allows us to see the septum directly. We then use the camera to guide us while we use a small surgical instrument to remove the septum, returning the divided cavity to a normal, single cavity.
If the uterine anomaly is a bicornuate uterus, unicornuate uterus, or a didelphic uterus, the malformation cannot be surgically resected because this would permanently damage the tensile strength of the uterine muscle. Instead, we counsel these patients about future reproductive risks, including risk for premature delivery, which requires additional monitoring by an obstetrician during pregnancy.
Why choose us for the treatment of a Müllerian anomaly?
Müllerian anomalies are uncommon conditions and they require management by an experienced multidisciplinary care team, including specialists from radiology, gynecology, urology, pediatric surgery, colorectal surgery as well as psychology, who help provide emotional support for our patients. At Children's Colorado, we have the experience managing these complex conditions and the multidisciplinary team to optimize the surgical outcome and psychosocial well-being of our teens.
The American Society for Reproductive Medicine (ASRM) provides multidisciplinary information, education, advocacy and standards in the field of reproductive medicine.
The Center for Young Women's Health (CYWH) is an educational entity that is committed to providing teen girls and young women with carefully researched health information, educational programs and conferences.
Next steps
-
Would you like to learn more about us?
Learn more about the Gynecology department -
Are you ready to schedule an appointment?
Schedule an appointment -
Do you have questions about your child’s condition?
720-777-2667



 720-777-0123
720-777-0123



